Influenza and diabetes
Seasonal influenza accounts for a significant proportion of excess winter mortality. Current policy in the UK and in many countries worldwide recommends annual flu vaccinations for patients with chronic conditions such as diabetes, though evidence to support such policies is limited.
Imperial College London used CPRD data to investigate the effectiveness of the influenza vaccine at reducing cardiovascular and respiratory hospital admissions and mortality in patients with type 2 diabetes. The study used linkages between CPRD GOLD primary care data, Hospital Episode Statistics (HES) and the Office for National Statistics (ONS) mortality data to look at admissions and death in 125,000 patients over a seven-year period. Influenza vaccination was associated with a reduction in the rate of hospital admissions for acute cardiovascular and respiratory disease and a reduction in all-cause mortality across the seven flu seasons.
The study has been widely reported within healthcare and mainstream media and supports current flu vaccination initiatives in the UK and beyond.
- Vamos EP, Pape UJ, Curcin V, Harris MJ, Valabhji J, Majeed A, Millett C. Effectiveness of the influenza vaccine in preventing admission to hospital and death in people with type 2 diabetes. CMAJ. 2016 Oct 4;188(14):E342-E351.
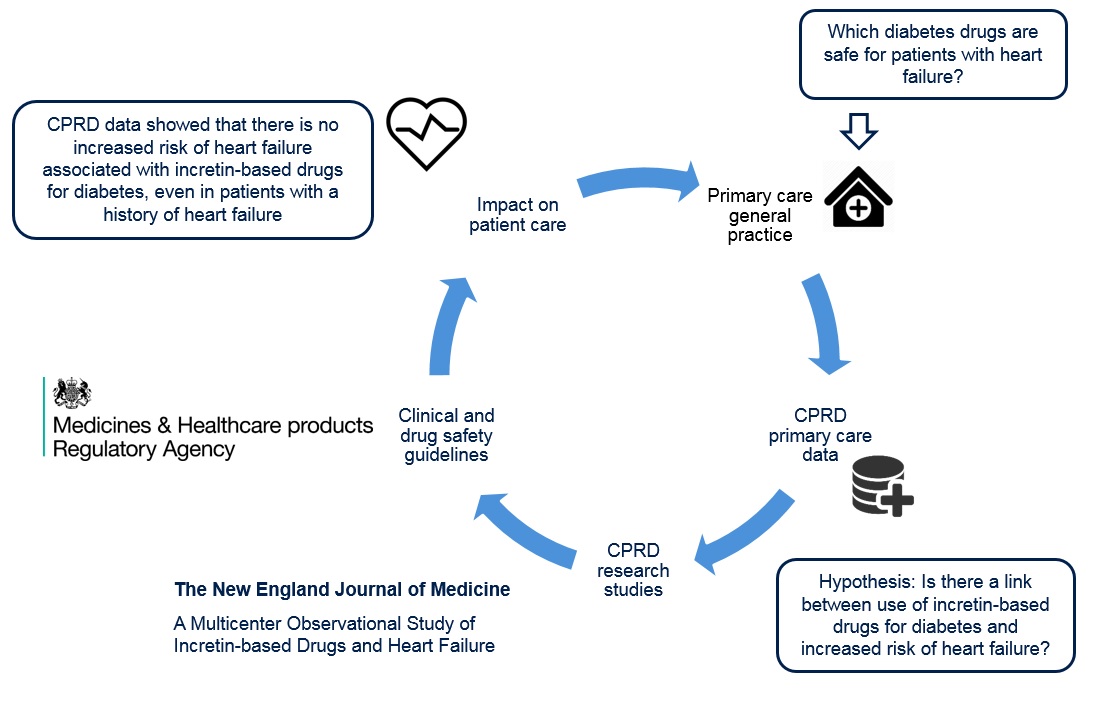
Incretin-based drugs and heart failure
Large multinational cohorts are vital to the investigation of drug safety.
CPRD data was used to investigate concerns over a possible link between antidiabetic, incretin-based drugs including dipeptidyl peptidase 4 (DPP-4) inhibitors and glucagon-like peptide 1 (GLP-1) analogues and an increased risk of heart failure in a cohort of 1.5 million diabetic patients from the UK, Canada and the United States.
This study was important in establishing the safety of a large, commonly used class of drugs for a disease which is on the rise globally. GLP-1 analogues were not associated with an increased risk of heart failure, compared with other commonly used combinations of antidiabetic drugs, even in patients with a history of heart failure.
- Filion KB, Azoulay L, Platt RW, Dahl M, Dormuth CR, Clemens KK, Hu N, Paterson JM, Targownik L, Turin TC, Udell JA, Ernst P; CNODES Investigators. A Multicenter Observational Study of Incretin-based Drugs and Heart Failure. N Engl J Med. 2016 Mar 24;374(12):1145-54. doi: 10.1056/NEJMoa1506115.
NICE guidelines and cancer diagnosis
Diagnosis of bladder cancer relies on the accurate assessment of common primary care symptoms. There is a need for clear and relevant guidelines to determine whether a patient’s symptom may warrant further investigation.
Researchers at the University of Exeter used CPRD data to identify and quantify the features of bladder cancer in primary care. Approximately 5,000 patients diagnosed with bladder cancer were matched with 22,000 controls to determine the positive predictive value of symptoms including haematuria (blood in the urine), urinary tract infection, abdominal pain, constipation and raised inflammatory markers.
Visible haematuria was found to be the most powerful predictor of bladder cancer and warrants further investigation. This study formed an important contribution to NICE guidelines on the diagnosis of cancer in primary care.
-
Shephard EA, Stapley S, Neal RD, Rose P, Walter FM, Hamilton WT. Clinical features of bladder cancer in primary care. Br J Gen Pract. 2012 Sep;62(602):e598-604.
You can view the bibliography of more than 3,000 research publications using CPRD data here.